S. No
|
NAME
|
UNIT
|
COVID ICU 1st DUTY
|
COVID ICU 2nd DUTY
|
104
|
P. Ruchitha Reddy
|
I
|
3-7-20
|
15 -7-20
|
105
|
Pippiri Sneha
|
II
|
3-7-20
|
15 -7-20
|
106
|
Polishetti Sreeja
|
III
|
4 -7-20
|
16 -7-20
|
107
|
Ponnam Nandakishore
|
IV
|
4 -7-20
|
16 -7-20
|
108
|
P.Venkata Jaswitha Sree
|
V
|
5 -7-20
|
17 -7-20
|
109
|
P. Manisha Reddy
|
VI
|
5 -7-20
|
17 -7-20
|
110
|
P. Geethika
|
I
|
6 -7-20
|
18 -7-20
|
111
|
Priyanka Vaddi
|
II
|
6 -7-20
|
18 -7-20
|
112
|
P. Chandana
|
III
|
7 -7-20
|
19 -7-20
|
113
|
P. Sai mahendra Reddy
|
IV
|
7 -7-20
|
19 -7-20
|
114
|
Ramavath Preesthi
|
V
|
8 -7-20
|
20 -7-20
|
115
|
Rangam Sandeep
|
VI
|
8 -7-20
|
20 -7-20
|
116
|
R. Rakesh Kumar
|
I
|
13 -7-20
|
21 -7-20
|
117
|
Aditya Rayilla
|
II
|
9 -7-20
|
21 -7-20
|
118
|
Rubeena Maheen
|
III
|
10 -7-20
|
22 -7-20
|
119
|
S. Sai Bharghavi
|
IV
|
10 -7-20
|
22 -7-20
|
120
|
Sai Kiran Kuna
|
V
| ||
121
|
Sai Pranavi V
|
VI
|
29-6-20
|
11 -7-20
|
122
|
S. Laasya Priya Sai
|
I
|
29-6-20
|
11 -7-20
|
123
|
Sambodhi Baid
|
II
|
30-6-20
|
12 -7-20
|
124
|
S. Roshini
|
III
|
30-6-20
|
12 -7-20
|
125
|
Rashi Seetha
|
IV
|
1 -7-20
|
9 -7-20
|
126
|
Sivani Chennupati
|
V
|
1 -7-20
|
13 -7-20
|
127
|
Soma Ram Reddy
|
VI
|
2 -7-20
|
14 -7-20
|
128
|
Sowmya Muthyala
|
I
|
2 -7-20
|
14 -7-20
|
Sunday, 28 June 2020
COVID Duty roster
Friday, 12 June 2020
Medicine E-log
Case history:
A 54 year old male patient came with Pain in the left side of the chest radiating to the back side since 2 days, difficulty in breathing since two days.
Patient was apparently asymptomatic 2 days back then he developed pain in the left side of chest all over, of stabbing type, which increased on inspiration, radiating to the left upper back.
Pain ass with difficulty in breathing in breathing (a sense of difficulty/strain during inspiration).
No history of shortness of breath.
No history of palpitations orthopnoea, PND, headache, burning micturition, vomiting loose stools, cough fever
Patient has complete loss of vision in both eyes since 10years patient was apparently asymptomatic 12 years back then he developed severe dragging type of pain in both the eyes for which he went to the doctor & was diagnosed to have glaucoma & was given medication which he used for 2 years with no improvement.
He was also operated 10 years back due to loss of vision, but there was no improvement in vision despite surgical intervention, but the pain had improved.
There is no history of HTN DM epilepsy asthma CVA CAD.
GRBS values on presentation turned out to be 740mg/dL
No history of headache, tingling sensation, numbness.
No history of decreased urine output.
History of burning sensation of both feet since 1 year.
On Examination the patient was conscious coherent and cooperative.
Febrile -100F
PR 104BPM
BP 160/100mmHg
RS BAE+ decreased breath sounds in left ISA coarse crepitations in lt IAA
CVS S1 S2 heard no murmurs
P/A soft non tender
Investigations:
On day 1:
ECG at presentation:
ABG at presentation showed slightly decreased levels of pCO2
Random blood sugars elevated- 740mg/dL
Complete urine examination showed elevated sugar levels
Urine was also tested was ketone bodies which turned out to be negative.
Hemogram shows increased TLC- 19,800 & increased neutophil levels
Renal functions were mostly normal, phosphorus levels were slightly elevated in the patient
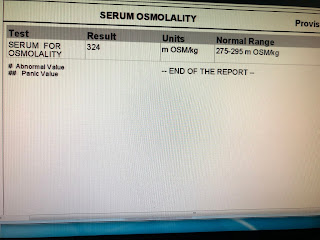
Serum osmolality was elevated- 324mOSM/kg
Chest X-ray on the first day shows slight effusion on the left lobe
Treatment:
9/6-
9pm- 538
10pm- 537
11- 472
10/6
12am- 437
1- 320
2- 266
3- 241
3:30- 229
4- 245
4:30- 274
5- 257
5:30- 317
6- 339 (1 unit of insulin in 39 parts of NS)
6:30- 435
7:30- 485
8:30- 446
10- 421
10:30- 413
11:30- 368
12:00- 431
12:30- 302
1:00- 346
1:30- 343
5pm- 316; 99.8F
7pm- 290
8pm- 1 unit subcutaneous insulin
10pm- 278
11/6 (GRBS Value in mg/dL)
12am- 238
2am- 179
4am- 164
6am- 157
8am- 271 (post breakfast)
9am- T.Glimiperide
10am- 264
12pm- 193; 101.2F
2pm- 203; 102.2F
4pm- 314
6pm- 319
8pm- 1/2 tab. Glimiperide
10pm- 361
12/6
1am- 268
4am- 254
6am- 238
8am- 238
9am- T.GLIMIPERIDE
10am-264
Fever chart:
Chest X-ray on day 4:
Culture sensitivity report showed klebsiella:
Chest radiograph and HRCT reports:
Pleural fluid- negative for malignant cytology;
Sediment smear was studied it showed scanty cellularity of Lymphocytes and few neutrophils only against eosinophilic proteinaceous background
Pleural sugar- 124mg/dL (elevated); pleural protein- 5g/dL, pleural LDH- 2240IU/L (elevated), pleural fluid ADA: 24U/L
Chest X-ray day 6:
USG- Chest shows thick septations and collapsed lung with minimal fluid
The ICD intervention would not be possible as there is less space
Consider breakage of loculations and septations through surgical intervention.
Bacterial culture negative for any aerobic bacteria.
Treatment:
1. Propped up position
2. Inj. piptaz 4.5gm/IV/TID day 7
3. Inj. Pan 40mg/IV/OD
4. T. Glimiperide BD (2.5mg - 1.5mg)
5. T. Ultracet 1/2 tab QID
6. BP PR RR hourly
7. GRBS 4th hourly
8. T vitC 1000mg/OD
9. T Telma 40mg/od
10. Inj neomol 1gm/iv infusion if temp >101F
11. Strict I/O charting
Diagnosis:
Left sided moderate loculated pleural effusion with left lower lobe pneumonic consolidation (exudative viral? Bacterial?)
Denovo HTN DM2
Cholelithiasis
Left sided moderate loculated pleural effusion with left lower lobe pneumonic consolidation (exudative viral? Bacterial?)
Denovo HTN DM2
Cholelithiasis
Monday, 8 June 2020
Daily Log
23rd may- Introduction to medicine internship (handovers and briefing)
24th may- Read up on CNS examination
25th may- ICU duty, learnt how to insert ryles tube
26th may- ICU Duty, read about antibodies in GBS and learnt how to intubate a patient
27th may- discussion about hypovolemic shock and metabolic acidosis treatment
28th may- differentiation of AKI from CKD, discussion about acute gastroenteritis
29th may- learned about quadriparesis causes and differential diagnosis for acute onset of weakness of limbs & functioning of NCS
30th may- discussion on thrombocytopenia and causes and relevance in an gastroenteritis patient
31st may- follow up on adenocarinoma patient developing epigastric pain and vomitings
1st june- referral of adenocarinoma patient to oncosurgeon and discussion of a possible treatment modality
2nd june- casualty duty, learned how to insert a foleys catheter
3rd june- hypokalemic periodic paralysis discussion on familial and autosomal dominant type of patterns and correction
4th june- Performed a pleural tap
5th june- Cause of pancytopenia in a HIV positive patient and necessity of a bone marrow biopsy to determine the root cause
6th june- counselled patient on hyperglycaemia compatible potassium rich foods, follow up on patient with exudative tap by checking up on the CT reports of chest to rule out any malignancy
7th june- read about Andersen-Tawil syndrome
8th june- compiled intern blogs and discussion on possible peripheral neuropathy
9th june- OPD day observed a case of possible HHS with hypertension and read about diagnostic difference of DKA and HHS
10th june- Gathered and complied history of patient with HHS and possible pneumonia
11th june- responsible for recording the session, a case of quadriparesis and HFPEF
12th june- witnessed a pleural tap, read functions of pseudocholinesterase and its deficiency
13th june- pleural fluid sample viewed and discussion on the cause of loculations and possible causes of pleural effusion
14th june- casualty duty observed a patient on ionotropes and read about the various uses and types of ionotropes and the receptors they act on
15th june- discussion on diabetes and it’s relation with recurrent urinary tract infections
16th june- OPD day, saw a patient of a temporo-occipital infarct and performed CNS examination
17th june- learned about scapulo-humeral reflex and sternal reflex
18th june- took patient for an ortho referral (suspecting patellar synovitis) and dermatology (diagnosis tinea corporis and cruris)
19th june- venous thrombosis patient with diplopia and blurring of vision taken to ophthalmology for consultation with the department
20th june- discussion about arterial and venous hemorrhages and discussion on circle of willis and various symptoms associated
21st june- read about CSVT
22nd june- Leave
23rd june- assisted in putting a ryles tube, took history of case of CVA and performed examination
24th june- acute pancreatitis patient observed and taken for ultrasound abdomen
25th june- discussed about differences in PSVT AVNRT and panic attacks & treatment, their ECG changes
26th june- ABCDEF type of management in acute pancreatitis & BISAP scoring discussed
27th june- Discussion on Acute gastroenteritis differences between bacterial and viral infections
28th june- Read about ECG changes in different types of heart blocks
29th june- Read about circle of willis and syndromes associated
30th june- OPD day, Saw a patient of hypertensive emergency and found out differences in hypertensive urgency and emergency
1st july- Attended to a patient of acute seizure episodes with right upper limb weakness with no CT brain findings
2nd july- Viewed a cushing syndrome patient and took complete history
3rd july- TIA occurring in hypertensive emergency chances and physiology of ECG wave conduction.
4th july-
24th may- Read up on CNS examination
25th may- ICU duty, learnt how to insert ryles tube
26th may- ICU Duty, read about antibodies in GBS and learnt how to intubate a patient
27th may- discussion about hypovolemic shock and metabolic acidosis treatment
28th may- differentiation of AKI from CKD, discussion about acute gastroenteritis
29th may- learned about quadriparesis causes and differential diagnosis for acute onset of weakness of limbs & functioning of NCS
30th may- discussion on thrombocytopenia and causes and relevance in an gastroenteritis patient
31st may- follow up on adenocarinoma patient developing epigastric pain and vomitings
1st june- referral of adenocarinoma patient to oncosurgeon and discussion of a possible treatment modality
2nd june- casualty duty, learned how to insert a foleys catheter
3rd june- hypokalemic periodic paralysis discussion on familial and autosomal dominant type of patterns and correction
4th june- Performed a pleural tap
5th june- Cause of pancytopenia in a HIV positive patient and necessity of a bone marrow biopsy to determine the root cause
6th june- counselled patient on hyperglycaemia compatible potassium rich foods, follow up on patient with exudative tap by checking up on the CT reports of chest to rule out any malignancy
7th june- read about Andersen-Tawil syndrome
8th june- compiled intern blogs and discussion on possible peripheral neuropathy
9th june- OPD day observed a case of possible HHS with hypertension and read about diagnostic difference of DKA and HHS
10th june- Gathered and complied history of patient with HHS and possible pneumonia
11th june- responsible for recording the session, a case of quadriparesis and HFPEF
12th june- witnessed a pleural tap, read functions of pseudocholinesterase and its deficiency
13th june- pleural fluid sample viewed and discussion on the cause of loculations and possible causes of pleural effusion
14th june- casualty duty observed a patient on ionotropes and read about the various uses and types of ionotropes and the receptors they act on
15th june- discussion on diabetes and it’s relation with recurrent urinary tract infections
16th june- OPD day, saw a patient of a temporo-occipital infarct and performed CNS examination
17th june- learned about scapulo-humeral reflex and sternal reflex
18th june- took patient for an ortho referral (suspecting patellar synovitis) and dermatology (diagnosis tinea corporis and cruris)
19th june- venous thrombosis patient with diplopia and blurring of vision taken to ophthalmology for consultation with the department
20th june- discussion about arterial and venous hemorrhages and discussion on circle of willis and various symptoms associated
21st june- read about CSVT
22nd june- Leave
23rd june- assisted in putting a ryles tube, took history of case of CVA and performed examination
24th june- acute pancreatitis patient observed and taken for ultrasound abdomen
25th june- discussed about differences in PSVT AVNRT and panic attacks & treatment, their ECG changes
26th june- ABCDEF type of management in acute pancreatitis & BISAP scoring discussed
27th june- Discussion on Acute gastroenteritis differences between bacterial and viral infections
28th june- Read about ECG changes in different types of heart blocks
29th june- Read about circle of willis and syndromes associated
30th june- OPD day, Saw a patient of hypertensive emergency and found out differences in hypertensive urgency and emergency
1st july- Attended to a patient of acute seizure episodes with right upper limb weakness with no CT brain findings
2nd july- Viewed a cushing syndrome patient and took complete history
3rd july- TIA occurring in hypertensive emergency chances and physiology of ECG wave conduction.
4th july-
INTERNS DAILY LOGS
INTERNS DAILY LOGS: 23rd MAY TO 22nd JULY
104
|
P. Ruchitha Reddy
|
I
| ||
105
|
Pippiri Sneha
|
II
| ||
106
|
Polishetti Sreeja
|
III
| ||
107
|
Ponnam Nandakishore
|
IV
| ||
108
|
P.Venkata Jaswitha Sree
|
V
| ||
109
|
P. Manisha Reddy
|
VI
| ||
110
|
P. Geethika
|
I
| ||
111
|
Priyanka Vaddi
|
II
| ||
112
|
P. Chandana
|
III
| ||
113
|
P. Sai mahendra Reddy
|
IV
| ||
114
|
Ramavath Preethi
|
V
| ||
115
|
Rangam Sandeep
|
VI
| ||
116
|
R. Rakesh Kumar
|
I
| ||
117
|
Aditya Rayilla
|
II
| ||
118
|
Rubeena Maheen
|
III
| ||
119
|
S. Sai Bharghavi
|
IV
| ||
120
|
Sai Kiran Kuna
|
V
| ||
121
|
Sai Pranavi V
|
VI
| ||
122
|
S. Laasya Priya Sai
|
I
| ||
123
|
Sambodhi Baiid
|
II
| ||
124
|
S. Roshini
|
III
| ||
125
|
Rashi Seetha
|
IV
| ||
126
|
Sivani Chennupati
|
V
| ||
127
|
Soma Ram Reddy
|
VI
| ||
128
|
Sowmya Muthyala
|
I
|
E-Log
E-Log |
Subscribe to:
Comments (Atom)